Medicaid Reform: HOAs
Even prior to Nevada’s expansion of Medicaid eligibility in 2013, state costs for Medicaid were rising unsustainably. Nevada’s Medicaid costs were already projected to grow faster than the most optimistic assumptions of the state’s gross domestic product.1
Following expansion, the number of Medicaid enrollees in Nevada was projected to rise from 268,000 in 2009 to about 802,000 by 2023.2 This forecast wound up underestimating growth slightly, as enrollment reached 904,158 in July 2022. The cost increases entailed by such enrollment growth make it essential that lawmakers reform Nevada Medicaid, if only to maintain the program’s affordability.
Key Points
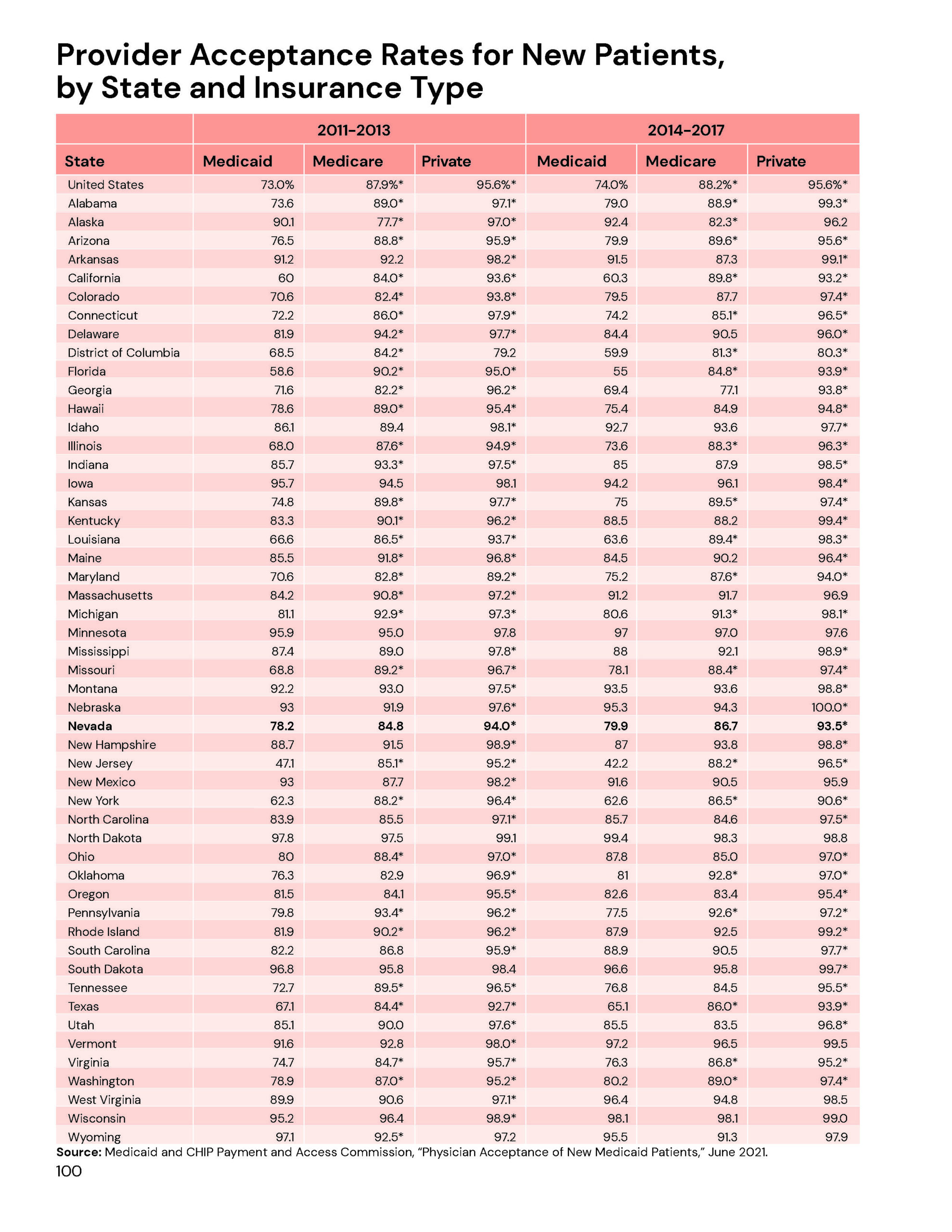
Access to insurance and access to care are not always synonymous. While Medicaid was intended to ensure access to health care for highly vulnerable populations, policymakers’ traditional approach to controlling Medicaid costs – reducing reimbursement rates of health care providers – works against this end. Given the very real prospect of being short-changed, many providers elect not to accept new Medicaid patients at all. Surveys from the Centers for Disease Control indicate that only 79.9% of Nevada doctors accept any new Medicaid patients, although a majority will not accept those with conditions costly to treat. By contrast, Nevada doctors accept 93.5% of privately insured new patients.3
As currently structured, Medicaid benefits may not be beneficial. Researchers at the University of Virginia have found, when it comes to health outcomes, it is better to be uninsured than on Medicaid. After examining a broad survey of surgical outcomes and adjusting for age and risk factors, their 2010 analysis finds that “surgical patients on Medicaid are 13% more likely to die than those with no insurance at all, and 97% more likely to die than those with private insurance.” 4
Cost inflation results from a lack of price sensitivity. Health care costs in the United States have skyrocketed in recent decades, as more and more health care has been funded through third-party payers. Individuals who do not directly bear a significant share of treatment costs are more likely to approve superfluous treatments. Those additional costs are then borne collectively – requiring universally higher premiums.
Price competition controls cost growth. The American health-care industry is suffering under a government-induced price system failure. Consumers have become insensitive to the prices of procedures and, as a result, do not shop among nor demand value from providers. This lack of consumer discipline allows providers to raise prices without restraint. In short, price signals in the health care industry no longer convey the information necessary for an efficient market.
Recommendations
Restructure Medicaid benefits around a “Healthy Adult Opportunity (HAO) Account.” The federal Centers for Medicare and Medicaid Services announced in 2020 that states could apply to implement an HAO program. An HAO demonstration allows states to make numerous changes to Medicaid programs, including work requirements or risk-adjusted premiums for non-mandatory enrollees. States may even be able to apply to incorporate Health Opportunity Accounts, as first authorized in 2005.
Health Opportunity Accounts are similar to health savings accounts, with states depositing Medicaid dollars into a beneficiary’s private account. The beneficiary can then use those dollars to purchase medical services directly. If the beneficiary uses Medicaid providers, the account is debited at standard Medicaid rates. For non-participating providers, the account is debited at a higher rate. When a beneficiary’s income rises and Medicaid eligibility ends, 25% of the balance remaining in the account returns to the state. The remainder is available to the beneficiary for the purchase of health coverage, job training or college tuition.
Health Opportunity Accounts cut through the bureaucracy and allow beneficiaries to purchase coverage directly. They also make beneficiaries price sensitive for health services, leading to more judicious behavior.
1 Jagadeesh Gokhale et al., “The Impact of ObamaCare on Nevada’s Medicaid Spending,” Nevada Policy Research Institute policy study, 2011.
2 Ibid.
3 Medicaid and CHIP Payment and Access Commission, “Physician Acceptance of New Medicaid Patients,” June 2021.
4 Damien LaPar et al., “Primary Payer Status Affects Mortality for Major Surgical Operations,” University of Virginia, 2010.